The landscape of modern medicine is undergoing a profound transformation, driven by innovations that promise to redefine therapeutic efficacy and patient outcomes. Among these, the breakthroughs in targeted drug delivery systems stand out as a particularly revolutionary frontier. This sophisticated approach moves beyond the conventional one-size-fits-all methodology of systemic drug administration, aiming instead to deliver therapeutic agents precisely to the site of disease with minimal off-target effects. The implications are staggering, offering the potential to enhance drug potency, reduce debilitating side effects, and ultimately, usher in a new era of personalized and precision medicine.
For decades, the primary challenge in pharmacology has been the inherent lack of specificity in how drugs interact with the body. When a medication is administered orally or intravenously, it circulates throughout the entire system, affecting not only the diseased cells but also healthy tissues. This non-discriminatory action is the root cause of the adverse side effects that often plague patients, from nausea and hair loss in chemotherapy to organ toxicity. The fundamental goal of targeted drug delivery is to overcome this hurdle by creating a "magic bullet"—a concept first envisioned by Paul Ehrlich over a century ago—that can seek out and destroy pathological cells while sparing healthy ones.
The recent surge in progress is largely attributable to concurrent advancements in nanotechnology, biomaterials science, and our deepening understanding of disease biology at the molecular level. Researchers are now engineering an array of ingenious carriers, predominantly at the nanoscale, designed to navigate the complex biological environment and unload their medicinal cargo at the designated target. These carriers include liposomes, which are synthetic, spherical vesicles that can encapsulate both hydrophilic and hydrophobic drugs; polymeric nanoparticles, offering tunable degradation rates and surface properties; and dendrimers, highly branched molecules with a precise structure that allows for controlled drug attachment.
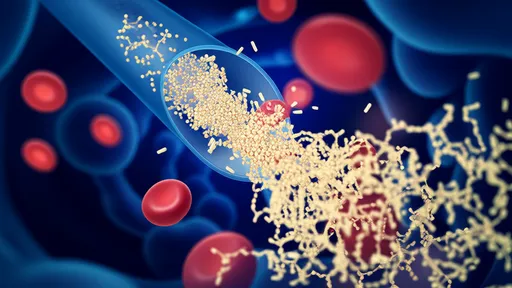
A critical breakthrough in this domain is the development of active targeting strategies. Unlike passive targeting, which relies on the enhanced permeability and retention effect—a phenomenon where nanoparticles tend to accumulate in tumor tissues due to their leaky vasculature—active targeting involves equipping drug carriers with specific ligands. These ligands, such as antibodies, peptides, or aptamers, act like homing devices. They are designed to recognize and bind exclusively to receptors or antigens that are overexpressed on the surface of target cells, such as cancer cells. This binding event triggers the internalization of the entire carrier into the cell, ensuring a highly localized and efficient drug release directly within the pathological environment.
Another transformative innovation is the creation of stimuli-responsive or "smart" drug delivery systems. These systems are engineered to remain inert and stable during circulation, only activating and releasing their payload upon encountering specific physiological triggers unique to the disease site. These triggers can be intrinsic, such as the slightly acidic pH commonly found in tumor microenvironments or inflamed tissues, or the elevated levels of certain enzymes like matrix metalloproteinases. Alternatively, they can be extrinsic, where release is controlled by an external stimulus applied by a clinician, such as light, heat, or a magnetic field. This level of spatiotemporal control was once the stuff of science fiction but is now becoming a tangible reality in laboratories worldwide.
The application of these technologies is making the most significant impact in the field of oncology. Chemotherapeutic agents are notoriously cytotoxic, and their non-specific nature causes severe collateral damage. Targeted delivery systems are changing this narrative. For instance, antibody-drug conjugates (ADCs) are a clinically validated class of targeted therapeutics where a monoclonal antibody, specific to a tumor antigen, is chemically linked to a potent cytotoxic drug. The antibody guides the conjugate to the cancer cell, where the drug is internalized and released, dramatically increasing the therapeutic index. Furthermore, nanoparticle-based platforms are being investigated to overcome multidrug resistance, a major cause of treatment failure, by bypassing efflux pumps that cancer cells use to expel chemotherapeutics.
Beyond cancer, targeted delivery is opening new avenues for treating a wide spectrum of diseases. In treating autoimmune disorders like rheumatoid arthritis, targeted systems can deliver anti-inflammatory drugs directly to inflamed joints, mitigating systemic exposure and its associated risks. For neurodegenerative diseases such as Alzheimer's, the major obstacle is the blood-brain barrier. Novel delivery systems are being designed to ferry therapeutic molecules across this formidable barrier to treat the root cause of the disease within the central nervous system. Even in gene therapy, viral and non-viral vectors are being refined to deliver genetic material with greater specificity and safety, correcting faulty genes at their source.
Despite the exhilarating progress, the path from laboratory bench to widespread clinical adoption is fraught with challenges. Scaling up the synthesis of these complex delivery systems to meet Good Manufacturing Practice standards for human use is a monumental task, requiring impeccable reproducibility and quality control. Furthermore, the long-term fate of these nanomaterials within the body—their biodegradation, potential for accumulation, and overall biocompatibility—requires thorough investigation to ensure patient safety. Regulatory agencies are now grappling with how to evaluate these multifaceted combination products, which blur the lines between drugs and devices.
Looking ahead, the future of targeted drug delivery is incredibly bright and points toward even greater personalization. The integration of theranostics—combining therapy and diagnostic imaging into a single agent—will allow clinicians to visualize the distribution of a drug carrier in real-time and monitor its therapeutic efficacy. We are also moving toward systems that can deliver multiple drugs in a sequential or synergistic manner, or even respond to the dynamic changes within a disease. As we continue to decode the intricate language of biology, the next generation of drug delivery systems will likely be autonomously intelligent, capable of making diagnostic decisions and executing therapeutic actions within the body without external intervention.
In conclusion, the breakthroughs in targeted drug delivery technology represent a paradigm shift in our approach to treating disease. By marrying the principles of engineering with the intricacies of biology, scientists are creating powerful new tools that promise to make treatments more effective, safer, and more humane. While hurdles remain, the relentless pace of innovation continues to bring us closer to the ultimate goal: delivering the right drug, to the right place, at the right time, for every patient.

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025